Semen Analysis: The semen sample is tested to identify the fertility rate of men and this process may require specimens to be collected in a sterile container.
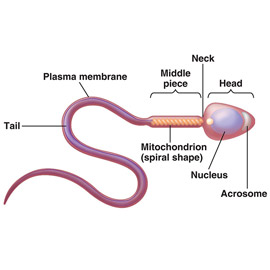
Morphology: This test does a complete evaluation of sperm structure which is done exclusively at Dr.Padmaja Fertility (IVF) Centre. We have facilitated the best predictor for sperm function.
Diagnostic Semen Wash: This laboratory procedure requires to extract sperm with re-suspension of the sperm in another solution.
This test is mandatory for IVF and GIFT procedures as well to identify other selective indications.
It may take 1 or 2 days of schedules with the lab and collection of specimen in a sterile container.
Studies: In a case where male factor concern is not explained by the referred tests, as the next part of the process, we take hormone evaluations and this include LH, FSH, testosterone, prolactin and thyroid studies.
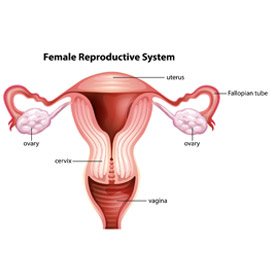
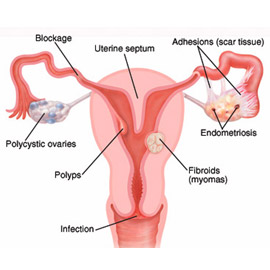
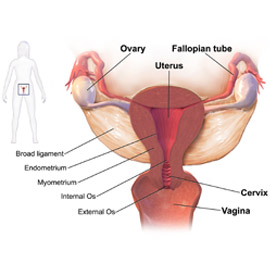
Post-Coital Test (PCT): Performs an evaluation of the sperm present in cervical mucus after intercourse to check for motility, quantity and survivability.
Antibody Testing: If there is any evidence of clumping of sperm on semen analysis or if no sperm is seen on PCT, the semen is evaluated for antisperm antibodies.
Biopsy: Patients with azoospermia may like to consider testicular biopsy with cryopreservation of any obtained sperm.